Putting patient welfare at the centre of innovation
Need an x-ray? Not possible – if you lived before 1895. How about laser eye surgery or a total hip replacement, surgical innovations of last century that have since bettered countless people’s quality of life?

The ethics of surgical innovation
Technological change is critical to improving health care. But innovation comes with potential costs. As surgeons ‘try something new’, often with the intent of improving an individual patient’s outcome, they run the risk of seriously harming their patients.
How can hospitals and surgeons safely introduce surgical innovations into practice?
The Applied Ethics team within the Macquarie University Ethics and Agency Research Centre is playing a key role in international efforts to address this crucial issue.
Patients first
New surgical technologies and techniques raise a host of ethical questions.
Are surgeons suitably trained in the innovation? How does the new approach affect patient care? Is it equitably available for all who need it? Can interested parties mitigate potential conflicts of interest? Have patients given fully informed consent?
Increasingly, the surgical profession is recognising the need for frameworks to assess whether a new technique or technology does actually serve the best interest of patients.
The stakes are high. We hear too many stories of the tragic consequences of surgical innovation gone wrong, such as when women were harmed through the untested use of mesh in pelvic operations.
But the complex nature of surgery makes surgical innovations more difficult to evaluate and regulate than other medical interventions like novel drug treatments.
What is innovative surgery?
Before Macquarie’s research, there was little agreement about how to define innovative surgery. This made it challenging for healthcare institutions to identify which interventions are innovative and therefore may require support.
 In response to these difficulties, Macquarie’s Applied Ethics team undertook research with surgeons, nurses and hospital managers. They developed a multifaceted definition of surgical innovation that distinguishes it from routine variations in clinical practice.
In response to these difficulties, Macquarie’s Applied Ethics team undertook research with surgeons, nurses and hospital managers. They developed a multifaceted definition of surgical innovation that distinguishes it from routine variations in clinical practice.
Importantly, the definition enables users to identify features of innovation before a surgeon applies a new technique or technology in the operating room.
From there, Professor Rogers (pictured) and colleagues Dr Katrina Hutchison, Professor Anthony Eyers, Associate Professor Mianna Lotz and Dr Brette Blakely developed and refined the Macquarie Surgical Innovation Identification Tool (MSIIT).
This ‘yes’/ ‘no’ checklist identifies potential innovations. If necessary, administrators can then implement support for the surgery or refer the planned procedure to an institutional research ethics review board. Download the MSIIT.
People preparing for surgery can also use the two MSIIT questions to expand on Question 4, ‘How many similar procedures have you done?’, of this online checklist of questions for your surgeon developed by the Royal Australasian College of Surgeons.
Safer processes
In many parts of the world, Macquarie’s work is improving the processes used by hospitals and surgeons to identify surgical innovation and, in turn, more safely manage risks.
The Royal College of Surgeons of England (RCS) incorporated Macquarie’s definition of surgical innovation and the MSIIT into their 2019 ‘Guide to Good Practice’. The RCS’s reach is extensive, with a global membership of nearly 30,000 surgeons, dental surgeons, and members of surgical and dental teams.
Rogers and Hutchison have worked closely with the Oxford-based international IDEAL Collaboration. IDEAL's goal is to improve surgical research. Macquarie's researchers have contributed to the latest IDEAL Framework, utilised by government agencies in several countries.
The Framework maps out the five-stage pathway essential to developing the evidence that a surgical innovation actually works.
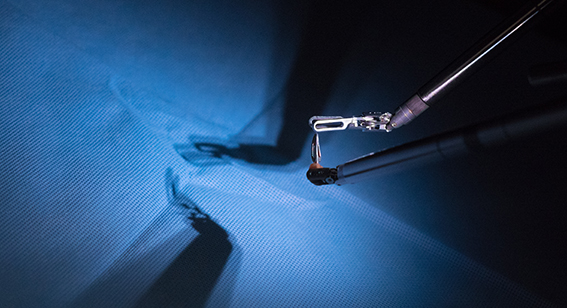 In recent years, the Framework has expanded to incorporate ethical guidance written by Professor Rogers, Dr Hutchison and Dr Angus McNair (Bristol University). This work builds on an approach to ethical issues in surgery developed by Rogers and Dr Jane Johnson. Dr Hutchison is also part of the IDEAL working group currently developing guidelines for evaluating surgical robots.
In recent years, the Framework has expanded to incorporate ethical guidance written by Professor Rogers, Dr Hutchison and Dr Angus McNair (Bristol University). This work builds on an approach to ethical issues in surgery developed by Rogers and Dr Jane Johnson. Dr Hutchison is also part of the IDEAL working group currently developing guidelines for evaluating surgical robots.
In Australia, Sydney’s Westmead Hospital was home to a pilot trial of the MSIIT in 2016 and 2017. The MSIIT is freely available to all hospitals in NSW and beyond.
Robotics, AI, VR .... At one time or another, most of us will likely benefit as surgeons continue to unveil new techniques and technologies. But more than that, we will also benefit from the work of Macquarie’s researchers who are helping to make innovative surgery safer for all.
Department of Philosophy
Macquarie University NSW 2109